The Hidden Risks of Heart Stents: What You Need to Know
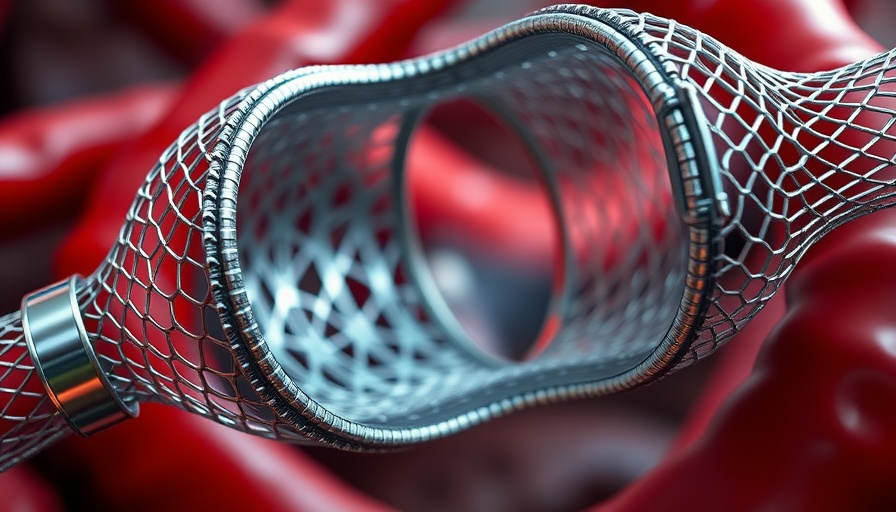
Every year, millions of individuals undergo stent placements to treat stable coronary artery disease (CAD), believing these procedures provide a safety net against heart attacks and chronic pain. However, recent insights suggest a stark contradiction between patient expectations and medical outcomes. As research reveals, angioplasty and stent placement may not only fail to prevent heart attacks but could also lead to serious health complications.
Understanding the Flaws in Current Practices
Stents are often utilized to restore blood flow; yet, the critical point is that the most dangerous plaques leading to cardiac events are not the ones targeted by stenting. Rather than aiding patients, PCI (percutaneous coronary intervention) can create an illusion of safety when, in reality, it does not prevent the underlying issues that cause heart attacks. Angioplasty looks beneficial on the surface, but as studies highlight, it might not assist patients like many believe.
How Common Are Complications?
Despite the low statistical chance of mortality or stroke related to stent placement, the fact that they are administered routinely poses a significant concern. The long-term consequences include potential heart failure, kidney injuries from the necessary dyes, and increase of silent mini-strokes which could contribute to cognitive decline. It’s startling to note that a vast number of patients may leave the procedure with new brain lesions—this risk raises questions about the overall benefit of such interventions.
Patient Perceptions vs. Medical Reality
One of the most troubling aspects of this issue is the vast difference in perception between medical professionals and patients. Many individuals hold the belief that stents will extend their life expectancy or prevent future heart issues, a conviction that is largely unfounded. Research suggests a considerable misinformation problem: over 70% of patients believe in the efficacy of stents, largely based on inadequate communication from physicians, who frequently prioritize procedure fees over patient education.
The Role of Communication in Patient Decision-Making
Effective communication is critical in healthcare, especially when discussing elective procedures. Unfortunately, many patients are not given the necessary information to make informed choices about their health. A mere 3% of conversations between doctors and patients include all essential elements of informed consent. This disconnect can lead to thousands choosing stenting procedures that may offer no real benefit, while missing out on impactful lifestyle changes that could improve their health.
Empowering Yourself: Questions to Ask Your Doctor
If you or someone you know is considering an angioplasty or stent placement, it’s essential to empower yourself with knowledge. Ask your doctor straightforward questions: What are the actual benefits of this procedure? Are there alternative treatments? What are the potential risks and side effects? Ensuring that you fully understand your options and the consequences of your decision is critical to navigating your heart health effectively.
Alternatives to Stenting: A Focus on Holistic Health
While stenting procedures are widely performed, it’s essential to consider alternatives that could yield better long-term health outcomes. Emphasizing a heart-healthy lifestyle—such as maintaining a balanced diet, engaging in regular exercise, managing stress, and avoiding smoking—can be far more effective in reducing the risks associated with heart disease. These lifestyle choices not only improve heart health but can also foster overall well-being.
In light of the information surrounding heart stents and their limited benefits, it’s crucial to assess your own healthcare journey critically. Take charge, ask the right questions, and consider all available options as you prioritize your heart health.
 Add Row
Add Row  Add
Add 




 Add Row
Add Row  Add
Add 


Write A Comment